Effective nursing care plans for Alzheimer’s patients require understanding of the disease, thorough assessments, realistic goal setting, and targeted interventions. This guide walks you through the essentials for managing Alzheimer’s, including the nursing care plan for Alzheimer’s, from cognitive assessments to setting care priorities and practical interventions.
Key Takeaways
-
Alzheimer’s disease is a progressive neurological disorder characterised by cognitive decline, with no known cure and a variety of risk factors influencing its onset and progression.
-
Comprehensive nursing care plans, including thorough assessments and realistic goal-setting, are crucial for managing Alzheimer’s patients and enhancing their quality of life.
-
Utilising assistive devices and creating a safe, familiar environment significantly improves the safety, well-being, and emotional support for both Alzheimer’s patients and caregivers.
Understanding Alzheimer's Disease

Alzheimer’s disease is a neurodegenerative disorder. It progressively impacts memory, cognition, and behaviour. As the leading cause of dementia, it accounts for approximately 70% of all dementia cases, profoundly impacting the lives of millions around the globe. Despite its prevalence, Alzheimer’s disease is not a normal part of ageing; it is a progressive neurological disorder that begins with subtle symptoms and gradually leads to significant cognitive decline.
Currently, there is no cure for Alzheimer’s disease, and while existing treatments can temporarily alleviate symptoms, they cannot halt the disease’s progression. Understanding the nature of this disease, its symptoms, and risk factors is crucial for effective care planning and management.
Understanding the intricate details of Alzheimer’s disease allows caregivers to better anticipate their loved ones’ needs and provide appropriate care.
Symptoms and Diagnosis
The onset of Alzheimer’s disease is often marked by minor memory lapses, such as forgetting recent conversations or events. As the disease progresses, patients may experience more pronounced confusion, communication deficits, and challenges in concentrating and processing information, along with secondary symptoms. These symptoms can significantly impact a patient’s daily life, so caregivers must recognise and address them promptly, ensuring they speak slowly and have ample time to provide support.
Diagnosing Alzheimer’s involves a thorough medical history review, cognitive tests, and sometimes brain imaging. Common tools used for cognitive assessment include the Mini-Mental State Examination (MMSE) and the Montreal Cognitive Assessment (MoCA).
Understanding the stages of Alzheimer’s, from preclinical to severe, helps in setting realistic care goals and preparing for the disease’s progression.
Risk Factors and Progression
Several risk factors contribute to the likelihood of developing Alzheimer’s disease. A family history of dementia, particularly with a first-degree relative, significantly increases this risk. Lifestyle choices, such as heavy alcohol consumption and smoking, also play a crucial role in the disease’s onset. Identifying these risk factors can help with early intervention and potentially slow the disease process.
Alzheimer’s disease progresses through four distinct stages: preclinical, mild, moderate, and severe. As the disease advances, cognitive and functional impairments become more pronounced, leading to increased dependency on caregivers. Understanding the disease progression helps caregivers prepare for the future and adapt their care strategies accordingly.
Key Components of a Nursing Care Plan for Alzheimer's

A comprehensive nursing care plan is crucial for effectively managing Alzheimer’s disease. These care plans help prioritise assessments, interventions, and goal-setting, ensuring that both short-term and long-term objectives are met. Tailoring interventions to individual patient needs allows caregivers to provide more personalised and effective care.
A well-structured nursing care plan should encompass thorough assessments, realistic goal setting, and targeted interventions. Education about Alzheimer’s disease can empower caregivers with the knowledge to handle daily challenges and improve the quality of life for their loved ones. This approach not only supports the patient but also provides a clear roadmap for caregivers to follow.
Assessment and Data Collection
Thorough assessment and data collection are the cornerstones of effective care planning for Alzheimer’s patients. Key components include:
-
Evaluating cognitive abilities
-
Assessing communication skills
-
Monitoring physical health
-
Regularly checking vital signs and physical health to adapt care plans to the patient’s changing condition
Regular assessment of safety concerns, such as the risk of falls and skin breakdown, is also necessary. Understanding the patient’s appearance, current self-care routine, and emotional state can provide valuable insights into their overall well-being and help tailor the nursing assessment care plan effectively, including aspects of personal care.
Setting Realistic Goals
Realistic and achievable goals are vital in managing Alzheimer’s disease. These goals should be tailored to the patient’s specific needs and capabilities, considering both short-term and long-term outcomes. Effective communication with the patient and their family is essential in establishing these goals and ensuring they are understood and supported.
Short-term goals might focus on daily tasks and immediate needs, while long-term goals could address overall quality of life and disease management. Setting clear, attainable objectives allows caregivers to provide structured and effective care, enhancing the patient’s well-being and expected outcomes in quality of life over a short period.
Common Nursing Diagnoses for Alzheimer's Patients
Accurate nursing diagnoses are essential for organising and prioritising care in Alzheimer’s nursing. These diagnoses help tailor interventions to the specific needs of the patient, improving the overall quality of care. Common nursing diagnoses for Alzheimer’s patients include impaired memory, risk for falls, and self-care deficits.
Understanding and addressing these diagnoses and related disorders enables caregivers to implement targeted interventions that enhance the patient’s daily functioning and safety. This approach ensures that the care provided is comprehensive and meets the unique needs of each patient.
Impaired Memory
Memory impairment is a hallmark of Alzheimer’s disease, presenting significant challenges for both a person with dementia and caregivers. Persistent forgetfulness can lead to increased confusion and difficulty in performing daily tasks. Implementing memory deficits and structured routines can help manage cognitive decline and enhance the patient’s ability to navigate their environment.
Addressing memory impairment is crucial in providing effective nursing care for Alzheimer’s patients. Simple interventions, such as using labels and signs, can aid in memory recall and reduce the frustration associated with memory loss. These strategies help maintain cognitive function and improve the patient’s quality of life.
Risk for Falls
Alzheimer’s patients face an increased risk of falls due to cognitive decline affecting their judgment and reasoning. Performing a fall risk assessment is essential to determine the level of risk and implement appropriate prevention strategies. Ensuring that bed rails, alarms, and call lights are accessible can significantly reduce the risk of falls.
Assessing environmental safety and managing mobility challenges are critical in preventing falls. Creating a safer environment helps minimise the risk of falls and ensures the safety and well-being of Alzheimer’s patients.
Self-Care Deficit
Self-care deficits are common in Alzheimer’s patients, affecting their ability to perform basic activities such as bathing, grooming, and feeding. Promoting self-care activities helps maintain the patient’s dignity, autonomy, and overall well-being. Caregivers should offer simple choices and assist with decision-making to support the patient’s independence.
Encouraging patients to perform as much of their self-care as possible boosts independence and self-esteem. Simple strategies, such as laying out clothing choices, can make daily tasks more manageable and less overwhelming for Alzheimer’s patients.
Nursing Interventions and Actions
 Nursing interventions for Alzheimer’s patients aim to promote function and independence while managing symptoms and enhancing quality of life. Patient education empowers both patients and caregivers to understand the disease and participate actively in care. Implementing systematic interventions at home can slow symptom progression and improve disease management.
Nursing interventions for Alzheimer’s patients aim to promote function and independence while managing symptoms and enhancing quality of life. Patient education empowers both patients and caregivers to understand the disease and participate actively in care. Implementing systematic interventions at home can slow symptom progression and improve disease management.
Assistive technology, such as medication reminders and smart home systems, plays a significant role in improving daily life for Alzheimer’s patients. These interventions help create a supportive environment that caters to the patient’s needs and promotes their well-being.
Enhancing Cognitive Function
Enhancing cognitive function is a primary goal in managing Alzheimer’s disease. Structured daily activities and familiar routines significantly reduce agitation and improve overall mood in Alzheimer’s patients. Clear labels and signs throughout the home aid memory recall and help patients navigate their environment.
Simple, repetitive tasks help maintain cognitive processing skills and promote mental engagement. Breaks or alternative activities can alleviate boredom and irritability, enhancing the patient’s overall well-being.
Managing Behavioural Symptoms
Managing behavioural symptoms such as aggression and agitation is crucial for Alzheimer’s patients. These symptoms can be triggered by stress, lack of sleep, or changes in environment or routine. A consistent daily routine and avoiding frustrating situations can prevent agitation and aggressive behaviour as well as hostile behaviours.
Limiting sensory stimuli and creating a structured, safe environment can decrease frustration and wandering behaviour. Installing wireless window and door alarms can also help prevent patients from wandering off unsupervised.
Providing Emotional Support
Emotional support reduces anxiety and promotes a sense of safety for Alzheimer’s patients. Consistent emotional reassurance and validating the patient’s feelings can significantly alleviate distress. Implementing these strategies fosters a positive environment that encourages autonomy and personal growth.
Goals should aim to maintain cognitive function and emotional well-being while enhancing social support to maintain independence. Robust emotional support helps patients feel more secure and valued, contributing to their overall mental health.
Utilising Assistive Devices and Technology
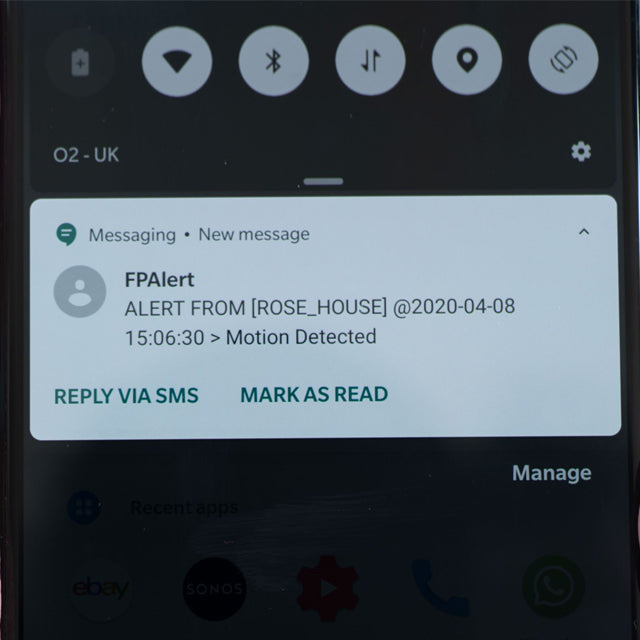
Assistive devices and technology play a crucial role in enhancing the safety and quality of life for Alzheimer’s patients. Devices like bed sensors and wearable trackers help monitor patients’ movements and ensure their safety. These technologies provide peace of mind to caregivers by allowing them to track and manage the patient’s whereabouts effectively.
Integrating assistive devices into the care plan creates a safer and more supportive environment for Alzheimer’s patients. These technologies aid in managing symptoms and improving overall care quality.
Bed Sensors and Alarms
Bed sensors are valuable tools for monitoring the movements of Alzheimer’s patients. These devices detect when a patient attempts to get out of bed and alert caregivers immediately, significantly reducing the risk of falls and wandering.
Bed sensors enhance caregiver awareness, creating a safer environment for Alzheimer’s patients. These devices are particularly useful in preventing wandering situations and ensuring the patient’s safety.
Wearable Trackers and GPS
Wearable trackers equipped with GPS technology are essential in monitoring the location of Alzheimer’s patients. These devices allow caregivers to locate wandering patients quickly, ensuring prompt assistance and enhancing safety.
Real-time location data provided by wearable GPS trackers offers peace of mind to caregivers, allowing them to monitor the patient’s movements and prevent wandering.
Supporting Family Caregivers
 Supporting family caregivers is crucial in the holistic care of Alzheimer’s patients. Family members often face overwhelming challenges due to the behavioural changes and communication difficulties associated with the disease. Appropriate strategies and resources help caregivers cope better and maintain their emotional and physical health.
Supporting family caregivers is crucial in the holistic care of Alzheimer’s patients. Family members often face overwhelming challenges due to the behavioural changes and communication difficulties associated with the disease. Appropriate strategies and resources help caregivers cope better and maintain their emotional and physical health.
Educational resources, support groups, and individualised care plans that consider caregiver preferences significantly enhance a person’s ability to provide effective care. Empowering caregivers with knowledge and support systems improves the overall care experience for both patients and their families.
Stress Management Techniques
Caregivers must manage their stress to provide consistent and compassionate care. Techniques include:
-
Balancing stimulation with rest during activities to prevent both the caregiver and the patient from feeling overwhelmed.
-
Offering reassurance to help manage patient hallucinations and emotional outbursts.
-
Using distraction techniques as a method to handle patient hallucinations and emotional outbursts and manage secondary symptoms.
Caregivers must have opportunities to express their concerns and feelings, which reduces anxiety and promotes emotional health. Responding calmly and validating the patient’s feelings helps manage catastrophic emotional responses and offer reassurance, creating a more supportive environment where they can communicate effectively.
Accessing Community Resources
Accessing community resources is vital for caregivers seeking support and respite. The local community Alzheimer’s Association and Alzheimer’s Society offer support groups that provide shared experiences and valuable coping strategies. Engaging with these groups can significantly alleviate the sense of isolation and provide practical advice for managing care.
Communities may offer professional counselling services tailored for caregivers, helping them navigate the emotional challenges of caregiving. Regular breaks and respite care are essential for caregivers to recharge and maintain their own health, ensuring they can continue to provide quality care for their loved ones.
Creating a Safe and Familiar Environment
A safe and familiar environment is essential for reducing agitation and aggression in Alzheimer’s patients. A calm and structured environment helps patients feel secure and supported, preventing confusion and erratic behaviours. The PLST model suggests modifying environmental demands to accommodate the declining cognitive and functional abilities of dementia patients.
Elements of care should include:
-
Ongoing education
-
Developing routines
-
Simplifying daily tasks
-
Implementing problem-solving strategies in a common form
Minimising clutter and noise prevents confusion and creates a more comfortable and safe living space for Alzheimer’s patients.
Home Modifications
Home modifications can significantly enhance the safety and comfort of Alzheimer’s patients. Simple adjustments include:
-
Removing or covering mirrors to prevent distress from unrecognised reflections
-
Using assistive devices
-
Maintaining a clutter-free environment reduces the risk of falls and other accidents.
Creating a supportive living space tailored to the patient’s needs helps maintain their dignity and independence. These modifications make daily tasks more manageable for a person living with challenges and supporting people less stressful for both patients and caregivers, promoting lifestyle changes that enhance overall well-being.
Daily Routine Planning
A consistent daily routine is crucial for Alzheimer’s patients. Routines reduce planning time and increase meaningful activities, benefiting both caregivers and patients. Adapting routines with creativity, flexibility, and problem-solving strategies is essential as the disease progresses.
Breaks or alternative activities can help maintain patients’ engagement and mood when they seem bored or irritable. While spontaneous activities can be enjoyable, they should be balanced with structured routines and rest periods to prevent anxiety and confusion.
Summary
Caring for elderly Alzheimer’s patients requires a multifaceted approach that includes understanding the disease, creating effective nursing care plans, managing symptoms, and providing robust support for caregivers. By focusing on these key areas, caregivers can enhance the quality of life for their loved ones and navigate the challenges of Alzheimer’s with greater confidence.
Empowering caregivers with knowledge, resources, and support systems is essential in this journey. By implementing the strategies and tips discussed in this guide, caregivers can provide compassionate and effective care, ensuring that Alzheimer’s patients live with dignity and comfort.
Frequently Asked Questions
What device can help caregivers monitor when Alzheimer's patients leave their beds?
Bed sensors specifically designed for Alzheimer's patients can effectively alert caregivers when a patient leaves their bed and does not return after a set period. This timely notification can greatly enhance the safety and monitoring of individuals with Alzheimer's.
Where can caregivers find quality assistive care devices for elderly loved ones?
Caregivers can find quality assistive care devices for elderly loved ones at Frequency Precision's online store. This resource offers a variety of options to meet individual needs.
What challenges do caregivers face when caring for loved ones with Alzheimer's?
Caregivers face significant challenges, including feelings of overwhelm, as they navigate the complexities of Alzheimer's, which affects their loved ones' memory, decision-making, and self-care abilities. These difficulties can lead to emotional and physical strain on the caregiver.
What is one major symptom of Alzheimer's that caregivers need to manage?
Wandering is a significant symptom of Alzheimer's that caregivers must effectively manage. It is essential to implement safety measures to prevent disorientation and ensure the well-being of the individual.
What safety measures should caregivers implement to prevent wandering?
To prevent wandering, caregivers should ensure their elderly loved one carries an ID, a GPS wearable tracker, and an emergency call button. These measures can significantly enhance safety and facilitate quick assistance if needed.