In our first article, Elaine Francis, a registered nurse with 18 years’ experience, writes about falls prevention and outcomes, and the challenges and drawbacks of fall prevention technology.

Falls: Outcomes and Prevention
Falls of all kinds have a high rate of poor outcomes, especially for older people. The older we get, the more at risk of falling we are, and the greater the risk of serious injury from those falls.[i] Older women in particular, with higher risk of osteoporosis, are at high risk of fractures. Fractures for men and women alike can be seriously debilitating, especially those with comorbidities[ii] – again more common as we age. The 1-year mortality rate following a hip fracture is high – between 14% and 58% in older people[iii], and for many of those who survive, quality of life is significantly reduced.[iv] Mobility, continence, skin integrity, appetite and mental health are all commonly adversely affected after a fractured neck of femur. Pressure damage, muscle wastage, and loss of independence are common. Clearly, avoiding falls is key to length and quality of life for many people.
Preventing Falls: Identifying Risk
Preventing falls takes a combination of multifactorial assessment and intervention tailored to the individual and setting[v]. A robust falls prevention training[vi] programme for staff can help empower carers to accurately assess and respond to risk. Ideally, face-to-face training should be available to informal carers too – at the very least, a run-down of falls prevention strategies and aids, and when and how to ask for help or further assessment. The attitude and perception of the individuals at risk can also have an impact on uptake of practical falls prevention – to begin to see oneself as an ‘at-risk’ person has connotations of old age and infirmity that may be difficult to accept.[vii]
Between 30% and 50% of people living in long-term care settings fall at least yearly[viii]. Staff may be able to identify those people at highest risk of falling and put measures in place to help keep them safe, and most formal carers have mandatory falls prevention training. Understanding the different mechanisms of falls is key to developing strategies for falls prevention; slips, trips and falls relating to an unsafe environment[ix] or inappropriate footwear[x] require a different approach to more complex falls associated with frailty, gait, cognitive impairment and continence issues.
Whether someone who is at high risk of falling is cared for in a formal setting or at home, it is not always possible or appropriate to watch them all the time – however high their risk of and from falling. The people at highest risk of falling are those who try to walk alone but are unsteady, and who are also unable to, or don’t remember to, call for help. This may be due to dementia, delirium, or a range of other cognitive, physical, or behavioural reasons – some people are simply reluctant to ask for support. Our risk of falling increases as we get older, and more than 30% of people aged over 65 fall more than twice a year[xi] – coinciding with our risk of serious injury from falls increasing as we age.
Falls Prevention Technology: Challenges and Drawbacks
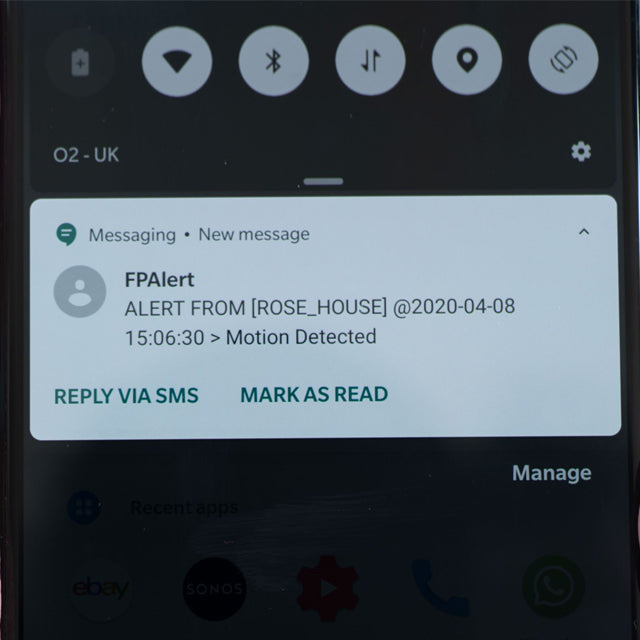
There have been a number of strategies developed over many years to tackle the risk of, and from, falls. Many of these have centred around finding ways of remotely alerting a carer that a person has risen from their bed or chair[xii], that they’ve opened doors, or sometimes even that they haven’t moved for a certain length of time. Increasingly sophisticated falls sensor technology is now joining the Internet of Things with connectivity inbuilt to enable remote alerts and monitoring. Relayed video technology is also available, which can support visibility for high-risk people. The care setting is an important consideration in falls prevention – the expectations on a formal care setting with adequate numbers of trained staff are different from a family member providing care at home. An alarm that alerts hospital staff to a patient’s movements is not necessarily the same alarm required to wake someone in the night when an elderly parent gets out of bed.
Falls prevention technology – motion sensors, pressure mats and alert systems – are a fantastic adjunct to nursing care, but have some inherent drawbacks – primarily that they respond to an incident as it happens. Ideally a carer will be able to attend quickly, and support the at-risk person to mobilise safely. However, falls can sometimes happen almost as soon as someone moves, so by the time a carer can respond to an alarm, it may be too late to prevent a fall. This is sometimes difficult to anticipate or prevent, but even in the worst case there is still clear value in carers being alerted and getting there almost immediately after a person has fallen. The prognosis after a long lie on the floor following a fall is very poor, and for a vulnerable person to be in a situation where they’re immobile, alone, injured and in pain for any length of time is unthinkable.
Interconnectivity in falls prevention technology has some compelling benefits – remotely monitoring vulnerable people can give families and carers peace of mind and help anticipate issues before they become incidents. There are some potential concerns over privacy, which need to be carefully weighed against the safety benefits; integrating security-by-design is an essential standard in any web-enabled technology, and consent and transparency are key in ethical close patient monitoring.
One Size Does Not Fit All
Falls have severe health repercussions, and contribute to a significant burden on resources for acute healthcare providers and community settings alike. Falls prevention strategies should, therefore, be as well-evidenced and valued as any other healthcare intervention. There are a number of clinical trials and research into the efficacy of existing and emerging falls prevention strategies; these range from small, single-venue studies to larger cohort trials[xiii]. There is not, however, a standardised trial template for all falls prevention.
A template for rigorous clinical testing would be as complex as the spectrum of situations in which someone falls. It would have to be adaptable or scalable for different care settings:
- at home with a relative providing ad hoc care
- assisted or supported living
- warden-controlled housing with or without carers on the premises
- residential or nursing care homes
- community or acute hospital settings[xiv]
…and every subset within those categories. The settings’ existing falls prevention practices could be presumed as a control.
The physical and cognitive abilities and needs of each individual at risk of falls is also relevant, and finally, the strategy or technology used; there are a huge number of different interventions which could reduce the impact of falls, such as simple advice[xv], physical alert technologies[xvi][xvii], vitamin supplements, exercise regimes[xviii], and cognitive behaviour therapy[xix] – to name a few.
The potentially catastrophic results of a fall would necessitate ethics committee approval before comparing different methods, but as there is currently little definitive evidence for one strategy over another, trialling different methods is unlikely to contravene ethical standards, and the long-term value of such a trial could be significant.
The benefits of falls prevention go beyond simply measuring how many falls occur using each method against a control; health and care is highly emotive, and some of the most important results are the least quantifiable. A comprehensive report on falls reduction should cover whether people feel generally safer with certain strategies. A reduction in stress and anxiety for loved ones, formal carers, and the people at risk is paramount. Studies which rely on self-reported anxiety levels aren’t always definitive, but could help answer important questions like whether those caring for their vulnerable relatives at home generally sleep better knowing that they would be reliably woken when needed – above all, whether people stay safe, feel safe, and live well.
About the Author
Elaine Francis is a registered nurse with 18 years' experience in healthcare.
She turned to medical writing to follow her passion for realistic and accessible medical communication, and is also currently working towards a master’s degree in the History of Medicine.
When Elaine isn’t writing or nursing, she spends her time telling her children to tidy up.
www.elainefrancis.com
[i] World Health Organization, World Health Organization. Ageing, & Life Course Unit. (2008). WHO global report on falls prevention in older age. World Health Organization. https://www.who.int/ageing/publications/Falls_prevention7March.pdf?ua=1
[ii] Hershkovitz, A., Polatov, I., Beloosesky, Y., & Brill, S. (2010). Factors affecting mortality of frail hip-fractured elderly patients. Archives of gerontology and geriatrics, 51(2), 113-116. https://doi.org/10.1359/jbmr.080702
[iii] Schnell, S., Friedman, S. M., Mendelson, D. A., Bingham, K. W., & Kates, S. L. (2010). The 1-year mortality of patients treated in a hip fracture program for elders. Geriatric orthopaedic surgery & rehabilitation, 1(1), 6–14. https://doi.org/10.1177/2151458510378105
[iv] Peeters, C. M., Visser, E., Van de Ree, C. L., Gosens, T., Den Oudsten, B. L., & De Vries, J. (2016). Quality of life after hip fracture in the elderly: a systematic literature review. Injury, 47(7), 1369-1382. https://doi.org/10.1016/j.injury.2016.04.018
[v] National Institute for Health and Care Excellence. (2013). Falls in older people: assessing risk and prevention. NICE. https://www.nice.org.uk/guidance/cg161
[vi] McKenzie, G., Lasater, K., Delander, G. E., Neal, M. B., Morgove, M., & Eckstrom, E. (2017). Falls prevention education: Interprofessional training to enhance collaborative practice. Gerontology & geriatrics education, 38(2), 232-243. https://doi.org/10.1080/02701960.2015.1127809
[vii] Whitehead, C. H., Wundke, R., & Crotty, M. (2006). Attitudes to falls and injury prevention: what are the barriers to implementing falls prevention strategies? Clinical Rehabilitation, 20(6), 536–542. https://doi.org/10.1191/0269215506cr984oa
[viii] Yoshida-Intern, S. (2007). A global report on falls prevention epidemiology of falls. Geneva: WHO.
[ix] Tse, T. (2005). The environment and falls prevention: Do environmental modifications make a difference?. Australian Occupational Therapy Journal, 52(4), 271-281. https://doi.org/10.1016/S0749-0690(18)30205-2
[x] Chase, C. A., Mann, K., Wasek, S., & Arbesman, M. (2012). Systematic review of the effect of home modification and fall prevention programs on falls and the performance of community-dwelling older adults. American Journal of Occupational Therapy, 66(3), 284-291. https://doi.org/10.5014/ajot.2012.005017
[xi] Dionyssiotis Y. (2012). Analyzing the problem of falls among older people. International journal of general medicine, 5, 805–813. https://doi.org/10.2147/IJGM.S32651
[xii] Vass, C. D., Sahota, O., Drummond, A., Kendrick, D., Gladman, J., Sach, T., ... & Grainge, M. (2009). REFINE (Reducing Falls in In-patient Elderly)-a randomised controlled trial. Trials, 10(1), 1-9. https://link.springer.com/article/10.1186/1745-6215-10-83
[xiii] Shorr, R. I., Chandler, A. M., Mion, L. C., Waters, T. M., Liu, M., Daniels, M. J., ... & Miller, S. T. (2012). Effects of an intervention to increase bed alarm use to prevent falls in hospitalized patients: a cluster randomized trial. Annals of internal medicine, 157(10), 692-699. https://doi.org/10.7326/0003-4819-157-10-201211200-00005
[xiv] Schwendimann, R., Bühler, H., De Geest, S. et al. Falls and consequent injuries in hospitalized patients: effects of an interdisciplinary falls prevention program. BMC Health Serv Res 6, 69 (2006). https://doi.org/10.1186/1472-6963-6-69
[xv] L Yardley, M Donovan-Hall, K Francis, C Todd (2006) Older people's views of advice about falls prevention: a qualitative study, Health Education Research, Volume 21, Issue 4. https://doi.org/10.1093/her/cyh077
[xvi] Subermaniam, K., Welfred, R., Subramanian, P., Chinna, K., Ibrahim, F., Mohktar, M. S., & Tan, M. P. (2017). The Effectiveness of a Wireless Modular Bed Absence Sensor Device for Fall Prevention among Older Inpatients. Frontiers in public health, 4, 292. https://doi.org/10.3389/fpubh.2016.00292
[xvii] Capezuti, E., Brush, B. L., Lane, S., Rabinowitz, H. U., & Secic, M. (2009). Bed-exit alarm effectiveness. Archives of gerontology and geriatrics, 49(1), 27–31. https://doi.org/10.1016/j.archger.2008.04.007
[xviii] Cumming RG. (2002) Intervention strategies and risk-factor modification for falls prevention. A review of recent intervention studies. Clinics in Geriatric Medicine. https://doi.org/10.1016/s0749-0690(02)00004-6
[xix] Cameron ID, Dyer SM, Panagoda CE, Murray GR, Hill KD, Cumming RG, Kerse N. (2018) Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database of Systematic Reviews. Issue 9. https://doi.org/10.1002/14651858.CD005465.pub4