The healthcare industry stands at the precipice of a digital revolution. With over 500,000 unique internet of medical things devices currently operating across healthcare settings worldwide, we’re witnessing an unprecedented transformation in how medical data is collected, analysed, and utilised to improve patient outcomes. The global IoMT in healthcare market, valued at £158 billion in 2023, represents far more than mere technological advancement—it signifies a fundamental shift towards proactive, personalised, and accessible medical care.
This comprehensive exploration examines how IoMT in healthcare is reshaping patient monitoring, clinical workflows, and medical innovation. From wearable devices that continuously track vital signs to smart hospitals equipped with interconnected medical equipment, the internet of medical things is creating an ecosystem where healthcare data flows seamlessly between patients, healthcare providers, and medical facilities.
Key Takeaways
The Internet of Medical Things connects medical devices to healthcare IT systems via internet networks, enabling remote patient monitoring and telemedicine services that were unimaginable just a decade ago. This technological integration has delivered measurable improvements across multiple healthcare metrics:
-
The global IoMT market reached £158 billion in 2023 and is projected to grow to £176 billion by 2026
-
IoMT devices include wearables, implantable devices, in-hospital equipment, and mobile health applications
-
The COVID-19 pandemic accelerated IoMT adoption by 300% in telehealth services during 2020-2022
-
Artificial intelligence and machine learning enhance IoMT functionality with 95% accuracy in health monitoring applications
-
Security challenges remain critical due to HIPAA regulations, with 82% of healthcare organisations reporting IoT device-targeted attacks
These statistics underscore both the tremendous potential and the pressing challenges that healthcare professionals must navigate when implementing IoMT technologies.
What is IoMT in Healthcare?
The Internet of Medical Things represents a specialised subset of the broader Internet of Things (IoT) ecosystem, focusing exclusively on medical device connectivity and healthcare applications. Unlike conventional IoT devices designed for consumer convenience, IoMT devices are engineered to collect data, monitor patients, and support clinical decision-making within strictly regulated healthcare environments.
IoMT encompasses the seamless connection of medical devices, healthcare applications, and IT systems through Wi-Fi networks and cloud computing platforms. This connectivity enables machine-to-machine communication without human intervention, allowing continuous data exchange between wearable devices, mobile devices, and healthcare systems. The technology supports everything from basic health monitoring to complex telemedicine consultations and automated clinical workflows.
The field gained momentum in the early 2010s alongside the miniaturisation of sensors and the expansion of wireless broadband infrastructure. Initial progress was driven by consumer fitness wearables, but the technology rapidly evolved as healthcare facilities recognised the potential for sensor-driven equipment to enhance patient care and operational efficiency. The pandemic served as a catalyst, accelerating the adoption and sophistication of IoMT infrastructure globally.
Today’s IoMT technology enables healthcare providers to access data from multiple sources simultaneously, creating comprehensive patient profiles that support personalised medicine approaches. This real-time connectivity between connected medical devices and healthcare providers’ network systems represents a fundamental shift from reactive to proactive healthcare delivery.
Types of IoMT Devices
The diversity of IoMT devices reflects the complex needs of modern healthcare delivery. These connected devices are categorised by their usage environment and clinical applications, each serving specific roles in the broader healthcare ecosystem.
In-Home IoMT Devices
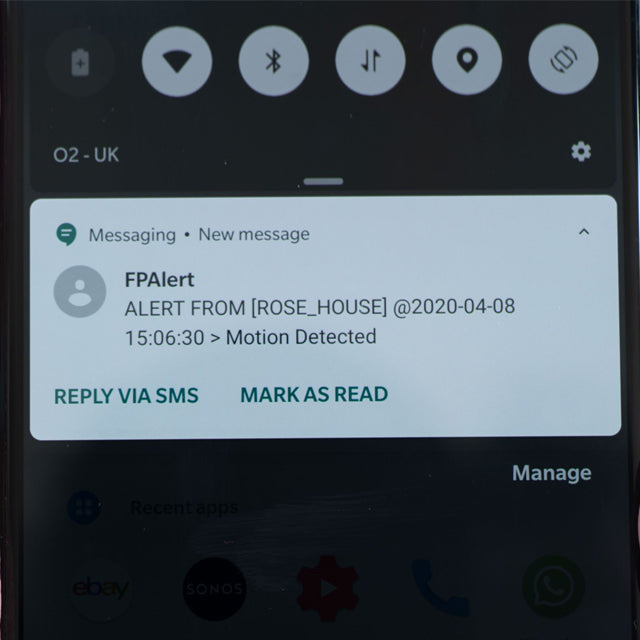
In-home IoMT devices have revolutionised chronic disease management and elderly care. Personal emergency response systems provide 24/7 monitoring for vulnerable populations, automatically alerting medical personnel when emergencies are detected. Remote patient monitoring devices enable patients to transmit medical data directly to their healthcare providers, reducing the need for frequent clinic visits.
Smart pill dispensers equipped with sensors ensure medication adherence whilst automatically updating healthcare systems with compliance data. Home diagnostic equipment, including blood pressure monitors and glucose meters, now features internet connectivity that allows real-time data sharing with healthcare professionals. Studies demonstrate that systematic use of in-home RPM devices reduces unnecessary patient hospitalisations by 30-40% whilst halving hospital readmissions for high-risk patients.
These devices represent a significant shift towards patient-centred care, empowering individuals to actively participate in their health management whilst maintaining a continuous connection with their healthcare providers.
Wearable IoMT Technology
Wearable sensors have evolved from simple fitness trackers to sophisticated medical monitoring systems. Consumer-grade devices like the Apple Watch Series 9, Fitbit Sense 2, and Samsung Galaxy Watch 6 provide continuous tracking of heart rate, activity levels, and sleep patterns. However, medical-grade wearables subject to rigorous regulatory approval offer far more precise monitoring capabilities.
Advanced wearable devices include ECG patches for continuous cardiac monitoring, neuromodulation units for neurological conditions, and smart contact lenses that monitor intraocular pressure or glucose levels. These devices achieve accuracy rates of 90-95% for heart rate and blood pressure monitoring, making them valuable tools for both patient self-management and clinical assessment.
The integration of artificial intelligence with wearable sensors enables predictive analytics that can identify potential health issues before symptoms become apparent. This proactive approach to health monitoring represents a paradigm shift from reactive treatment to preventive care.
Mobile IoMT Applications
Smartphone-based health applications leverage Near Field Communication (NFC) and radio frequency identification technologies to create comprehensive health management platforms. These mobile applications enable real-time communication between patients and healthcare providers whilst integrating with networked medical equipment in homes and clinical settings.
Notable applications include MySugr for diabetes management and KardiaMobile for mobile ECG acquisition. These platforms demonstrate how mobile devices can serve as central hubs for collecting data from multiple IoMT devices, creating unified patient health profiles that support informed clinical decision-making.
The proliferation of mobile health applications has democratised access to healthcare monitoring, particularly benefiting rural and underserved populations who may have limited access to traditional medical facilities.
In-Hospital IoMT Systems
Smart hospitals represent the pinnacle of IoMT integration, where interconnected systems create seamless clinical workflows. Smart infusion pumps connected to analytics dashboards provide real-time medication administration monitoring, whilst sensor-equipped hospital beds track patient movement and vital signs continuously.
Hospital-wide RFID systems monitor the location and status of medical equipment, supplies, and personnel, reducing inefficiencies and improving resource allocation. These asset management systems can reduce equipment misplacement by 25-35%, directly impacting operational costs and patient care delivery.
Advanced surgical systems, such as the Da Vinci robotic platform, exemplify how connected medical devices enhance precision and outcomes in complex procedures. These systems integrate multiple data streams to support real-time decision-making during critical interventions.
Public IoMT Infrastructure
Community-based IoMT infrastructure extends healthcare monitoring beyond traditional clinical settings. Point-of-care kiosks in pharmacies and community centres provide accessible health screening services, whilst connected automated external defibrillators (AEDs) in public spaces enhance emergency response capabilities.
These public health monitoring stations are particularly valuable in rural areas where access to healthcare facilities may be limited. They create networks of care that extend the reach of healthcare services whilst generating valuable population health data.
Benefits of IoMT in Healthcare
The implementation of IoMT in healthcare delivers measurable improvements across multiple dimensions of care delivery and operational efficiency. Enhanced patient outcomes result from continuous real-time monitoring that enables early detection of health deteriorations and timely interventions.
Research indicates potential annual healthcare savings of £300 billion by 2025, primarily through reduced hospital admissions and early intervention for chronic diseases. Hospitalisation rates have declined by approximately 40% in chronic disease populations using systematic remote patient monitoring, demonstrating the technology’s capacity to shift care from reactive to preventive models.
The technology significantly improves healthcare accessibility, particularly for rural and underserved populations. Patients can access specialist consultations and continuous monitoring services regardless of geographical constraints, reducing health disparities and improving equitable access to quality care.
IoMT supports personalised medicine by enabling continuous data collection that reveals individual health patterns and responses to treatments. This granular level of health data allows healthcare providers to tailor interventions to each patient’s specific needs and circumstances.
Early disease detection capabilities have shown particular promise, with some studies indicating 20-30% improvements in survival rates for conditions identified through continuous monitoring compared to traditional periodic check-ups.
AI and Machine Learning Integration
The convergence of artificial intelligence with IoMT technology has created unprecedented opportunities for intelligent healthcare delivery. Machine learning algorithms process vast streams of IoMT data to identify patterns that would be impossible for human analysis to detect, achieving accuracy levels of 95% or higher in specific diagnostic and risk stratification tasks.
Natural Language Processing enhances clinical documentation by automatically extracting relevant information from patient communications and medical records. This automation reduces the administrative burden on healthcare professionals while ensuring comprehensive data capture.
Deep learning applications in medical imaging analysis complement IoMT device data to provide holistic patient assessments. When combined with continuous monitoring data from connected devices, these systems can predict health deteriorations with remarkable accuracy, enabling proactive interventions.
Industry platforms such as IBM Watson Health, Google’s DeepMind, and Microsoft Healthcare Bot are scaling intelligent IoMT solutions across healthcare systems worldwide. These platforms demonstrate how artificial intelligence can transform raw sensor data into actionable clinical insights.
IoMT Applications in Specific Medical Conditions
Cardiac Monitoring and Cardiovascular Care
Continuous cardiac monitoring through IoMT devices has revolutionised cardiovascular care delivery. Wearable ECG monitors and smartwatches provide 24/7 rhythm tracking, with certain devices demonstrating 92% accuracy in identifying atrial fibrillation—a condition that often goes undetected during routine clinical visits.
The integration of cardiac monitoring data with telemedicine platforms enables remote cardiac rehabilitation programmes and proactive care management. Healthcare systems like the Mayo Clinic have demonstrated significant improvements in patient outcomes through the systematic implementation of connected cardiac monitoring systems.
Blood pressure monitoring systems with wireless connectivity allow for trend analysis that reveals patterns invisible in single-point measurements, supporting more accurate hypertension management and cardiovascular risk assessment.
Diabetes Management
Continuous glucose monitoring systems represent one of the most successful applications of IoMT technology in chronic disease management. Devices like the Dexcom G7 and FreeStyle Libre provide automated, high-frequency glucose readings that eliminate the need for frequent finger-stick testing.
Smart insulin pens integrated with algorithm-driven decision support systems help patients optimise their insulin dosing based on real-time glucose trends and predictive analytics. Studies demonstrate an average 1.2% reduction in HbA1c levels among users of integrated IoMT diabetes management systems.
The seamless integration of glucose data with smartphone applications and healthcare provider systems creates comprehensive diabetes management ecosystems that support both patient self-care and clinical oversight.
Respiratory Health and COVID-19 Monitoring
Connected inhalers for asthma and COPD management automatically log usage patterns and environmental triggers, providing healthcare providers with detailed insights into patient compliance and symptom patterns. This data enables personalised treatment adjustments and proactive intervention strategies.
Remote pulse oximetry monitoring became essential during COVID-19, enabling home-based monitoring of oxygen saturation levels for infected patients. This approach reduced hospital admissions whilst ensuring timely intervention when clinical deterioration occurred.
Remote patient monitoring for pulmonary patients has delivered a 60% reduction in emergency room visits for acute exacerbations, demonstrating the technology’s capacity to prevent complications through early detection and intervention.
Challenges and Limitations of IoMT
Security and Privacy Concerns
The proliferation of connected medical devices has created unprecedented cybersecurity challenges for healthcare organisations. With 82% of healthcare facilities reporting cyberattacks targeting IoT devices, the protection of sensitive patient data has become a critical operational priority.
Healthcare data transmitted through IoMT networks must comply with stringent regulations, including HIPAA in the United States and GDPR in the United Kingdom. These frameworks mandate specific encryption protocols, access controls, and audit trails that can be challenging to implement across diverse device ecosystems.
Data breaches involving medical information can have devastating consequences for both patients and healthcare providers, making robust cybersecurity measures essential rather than optional. The interconnected nature of IoMT systems means that a single compromised device can potentially provide access to entire healthcare networks.
Technical and Operational Challenges
Interoperability remains a significant obstacle to IoMT implementation, as many medical device manufacturers use proprietary communication protocols that don’t integrate seamlessly with existing healthcare systems. This fragmentation can create data silos that limit the technology’s potential benefits.
Infrastructure requirements for comprehensive IoMT deployment can be substantial, with large healthcare systems typically investing £10-50 million in hardware, software, secure network infrastructure, and staff training. Battery life limitations in wearable devices and the need for reliable internet connectivity add additional operational complexities.
Firmware and software updating for embedded medical devices presents ongoing challenges, particularly regarding cybersecurity patching. The critical nature of medical equipment means that updates must be thoroughly tested to ensure they don’t compromise device functionality or patient safety.
Regulatory and Compliance Issues
The regulatory approval process for medical-grade IoMT devices involves extensive clinical validation, documentation, and quality assurance requirements. FDA approval in the United States or CE marking in Europe and the UK can take years and require substantial financial investment.
Insurance reimbursement for IoMT services often lags behind technological innovation, as healthcare payment systems adapt slowly to new monitoring and treatment modalities. This delay can limit patient access to beneficial technologies and slow adoption rates among healthcare providers.
Quality control and device validation requirements necessitate continuous monitoring and reporting, adding administrative overhead to healthcare operations while ensuring patient safety and regulatory compliance.
IoMT vs Traditional IoT: Key Differences
The distinction between IoMT and traditional IoT devices extends far beyond their application domains. Healthcare-focused devices operate under stringent regulatory oversight that doesn’t apply to consumer IoT products, reflecting the life-critical nature of medical applications.
|
Aspect |
IoMT |
Traditional IoT |
|---|---|---|
|
Regulatory Compliance |
HIPAA, FDA, CE Mark, GDPR |
Minimal oversight |
|
Data Sensitivity |
Protected health information |
General user data |
|
Security Requirements |
Medical-grade encryption and access controls |
Standard cybersecurity measures |
|
Professional Oversight |
Healthcare professionals and clinical teams |
End-user management |
|
Integration Requirements |
Electronic health records and clinical systems |
Consumer applications and platforms |
|
Reliability Standards |
Life-critical system specifications |
Consumer-grade reliability |
This fundamental difference in operational requirements means that IoMT devices must meet substantially higher standards for reliability, security, and clinical validation than their consumer counterparts.
Future Trends and Innovations
The IoMT market is projected to reach £254 billion by 2028, driven by advancing communication technologies and expanding clinical applications. The integration of 5G networks will enable ultra-low latency communications essential for real-time surgical guidance and emergency response systems.
Edge computing represents a significant advancement in IoMT capabilities, enabling data processing at or near the device level. This approach reduces latency, improves reliability, and enhances privacy by minimising the transmission of sensitive data across networks.
Blockchain technology is increasingly being piloted for secure, tamper-resistant exchange of health data between healthcare providers and patients. This distributed approach to data management could address many current concerns about data ownership and security.
Nanotechnology integration promises to further miniaturise diagnostic capabilities, with graphene-based biosensors under development for continuous, non-invasive monitoring of multiple biomarkers simultaneously. These advances could enable early detection of diseases at the molecular level.
Virtual and augmented reality technologies, when combined with IoMT data streams, are creating new possibilities for medical education, surgical training, and therapeutic interventions. These immersive technologies enhance the value of collected data by providing intuitive interfaces for data interpretation and clinical decision-making.
Implementation Strategies for Healthcare Organisations
Successfully implementing IoMT technology requires comprehensive strategic planning that addresses technical, financial, and operational considerations. Healthcare organisations typically begin with pilot programmes to validate return on investment and develop integration templates before system-wide deployment.
Budget planning should account for the full lifecycle costs of IoMT implementation, including initial hardware and software investments, ongoing maintenance, staff training, and system upgrades. Large health systems commonly invest £10-50 million for comprehensive IoMT integration across multiple facilities.
Staff training and change management are critical success factors, as healthcare professionals must adapt to new workflows and data management processes. Successful implementations typically include extensive training programmes and gradual rollout schedules that allow staff to adapt to new technologies progressively.
Partnership strategies with established technology vendors can accelerate implementation timelines and reduce technical risks. Major cloud platforms like Microsoft Azure and Google Cloud offer specialised healthcare solutions that provide secure, compliant infrastructure for IoMT deployment.
Performance measurement frameworks should be established before implementation to track return on investment, patient outcomes, and operational efficiency improvements. Key metrics typically include reduced admission rates, improved patient satisfaction scores, and decreased care delivery costs.
Case studies from leading healthcare institutions like Johns Hopkins and the Mayo Clinic demonstrate that systematic IoMT implementation can deliver substantial improvements in clinical workflows, patient engagement, and health outcomes when properly planned and executed.
Frequently Asked Questions
What is the difference between IoMT and regular IoT devices?
IoMT devices are specifically designed for healthcare applications and must meet stringent regulatory requirements, including FDA approval and HIPAA compliance. They integrate with electronic health records and support clinical decision-making, whilst regular IoT devices focus on consumer convenience without medical oversight or regulation.
How secure are IoMT devices for patient data?
IoMT device security varies significantly by manufacturer and implementation. Medical-grade devices must comply with healthcare data protection regulations and typically employ advanced encryption, secure authentication, and regular security updates. However, security assessments remain critical as cyber risks continue to evolve.
What are the main benefits of IoMT for patients?
Patients benefit from continuous health monitoring, early disease detection, improved chronic disease management, and enhanced access to healthcare services. Remote patient monitoring enables proactive care that can prevent complications and reduce hospital admissions by up to 40% for certain conditions.
How much does it cost to implement IoMT in a hospital?
Implementation costs for large healthcare systems typically range from £10-50 million, including hardware, software, network infrastructure, staff training, and change management. Smaller healthcare facilities may implement focused IoMT solutions for substantially lower investments.
Can IoMT devices replace traditional medical equipment?
IoMT devices typically complement rather than fully replace traditional medical equipment. They enhance existing capabilities through connectivity and data integration whilst maintaining the core functionality of conventional medical devices. Integration with smart devices creates more comprehensive monitoring and care delivery systems.
What regulations govern IoMT devices?
IoMT devices must comply with multiple regulatory frameworks, including HIPAA for data protection, FDA approval for medical devices in the United States, and CE marking for European markets. International regulatory differences can affect global deployment strategies and device availability.
How does IoMT improve chronic disease management?
IoMT enables continuous monitoring of chronic conditions, automated medication adherence tracking, and real-time data sharing with healthcare providers. This comprehensive approach has been shown to reduce hospitalisations by 40% and improve clinical outcomes through early intervention and personalised treatment adjustments.
What are the biggest challenges in IoMT adoption?
Primary challenges include cybersecurity risks, interoperability issues between different manufacturers’ devices, high implementation costs, regulatory compliance requirements, and the need for comprehensive staff training. Healthcare organisations must address these challenges systematically to achieve successful IoMT deployment.
The Internet of Medical Things represents a transformative force in modern healthcare delivery, offering unprecedented opportunities to improve patient outcomes while reducing costs and enhancing accessibility. As the technology continues to evolve, healthcare organisations that embrace IoMT innovation position themselves at the forefront of patient-centred care delivery. The convergence of artificial intelligence, advanced sensors, and secure connectivity creates possibilities for healthcare transformation that were unimaginable just a decade ago. Success in this rapidly evolving landscape requires strategic planning, robust security measures, and a commitment to continuous adaptation as IoMT technologies advance.